Breast cancer risk estimates for individual women vary substantially depending on which risk assessment model is used, and women are likely receiving vastly different recommendations depending on the model used and the cutoff applied to define “high risk,” according to a new study from the University of California-Los Angeles (UCLA). The study appears online in Journal of General Internal Medicine.
Current incidence rates indicate that about one in eight women born in the United States today will develop breast cancer at some time during her life. The risk increases with age.
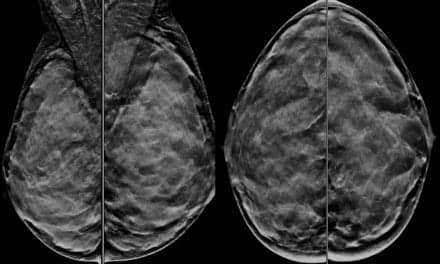
As precision medicine evolves in healthcare, breast cancer risk models are increasingly used to identify women who would benefit from medicines to reduce the risk of breast cancer as well as supplemental MRI screening. Easy-to-use risk models are readily available online and women are often given a risk estimate on their screening mammogram reports. An important question is how accurate are those models?
In 2019, the U.S. Preventive Services Task Force recommended that clinicians offer risk-reducing medications, such as tamoxifen, raloxifene, or aromatase inhibitors, to women who are at high risk for breast cancer in the next five years and at low risk for adverse medication effects.
While previously, a five-year risk cutoff of 1.67% was established, the task force recommended a new, higher fiver-year risk cutoff of 3%. And while current breast cancer risk assessment tools work well at a population level, little attention has been paid to how they perform at an individual level or to the variation in risk estimates for the ≥ 3.0% five-year threshold at the level of the individual.
The current study included more than 31,115 women who were part of the Athena Breast Health Network, a statewide quality improvement initiative across the University of California medical and cancer centers. It focused on three commonly used risk assessment models: the Breast Cancer Risk Assessment Tool (BCRAT, also called the Gail model), the Breast Cancer Surveillance Consortium (BCSC), and the International Breast Intervention Study (IBIS, also called the Tyrer-Cuzick model).
Investigators found when using a threshold of ≥ 1.67%, more than 21% of women were classified as high risk for developing breast cancer in the next five years by one model but average risk by another model.
When using a ≥ 3.0% threshold, more than 5% of women had disagreements in risk severity between models. If all three models were used, almost half of women (46.6%) were classified as high risk by at least one model. Because most women will not be diagnosed with breast cancer within five years, the authors say many women would be incorrectly classified as high risk.
“This study highlights the risk of a blanket approach to using risk prediction models to inform individual-level medical screening and treatment decisions,” says Joann Elmore, MD, MPH, the paper’s senior author and a professor of medicine in the division of general internal medicine and health services research at the David Geffen School of Medicine at UCLA. “All three of the models we looked at had similar accuracy at the population level, but in our analyses, there was marked disagreement between who was identified as ‘high risk’ by all three models.”
The authors say their findings highlight the tradeoff of sensitivity and inaccurate classification of “high risk” when using the two different thresholds currently recommended. For example, when using the ≥ 1.67% cutoff for considering chemoprevention, about half of the women diagnosed with a future breast cancer might be correctly identified as high risk, yet many more women would be falsely classified as high risk.
While using the more conservative ≥ 3.0% cutoff would lead to far fewer women incorrectly classified as high risk, most of the women with a future breast cancer diagnosis would be missed.
The study has some limitations. For example, the cohort was drawn from women enrolled in a longitudinal screening study. And although the authors had extensive risk factor data on many participants, some family history was missing as was data on polygenetic risk scores.
The authors point out that newer risk models are being developed that include information on breast cancer susceptibility genes and genetic susceptibility variants, which may improve predictability. Meanwhile several recent studies suggest that quantitative imaging biomarkers and artificial intelligence algorithms might also supplement or supplant the current, subjective clinical risk assessment tools.