“Hindsight is 20/20,” one often hears in the context of a tendency to evaluate past choices more clearly considering new information. But the perfect “20/20” score, referring to a measure of visual acuity, acknowledges a well-known psychological phenomenon called “hindsight bias.” Hindsight bias causes people to overestimate their own ability in predicting an outcome when, in fact, they couldn’t have predicted it accurately.
Hindsight bias can come in various forms. Visual hindsight bias, for example, is a type of bias where prior knowledge about an image improves our perception of it. It gives the impression that the improved perception comes from visual cues alone and has little to do with prior information.
While visual hindsight bias can impact people from all walks of life, it is particularly problematic for medical professionals, especially radiologists. In fact, breast radiologists have been sued in the past for missing a tumor in the early-stage images of cancer. In contrast, a radiologist may also claim that they can indeed see the tumor, a claim just as much subject to visual hindsight bias. As such events are common among radiologists, visual hindsight bias could entail serious legal consequences for them.
In a recent study published in the Journal of Medical Imaging (JMI), a team of researchers from the U.S. explored the extent to which expert radiologists experience visual hindsight bias when reading mammograms. They focused specifically on breast radiologists as mammography is one of the fields within radiology where medical professionals are most sued for negligence.
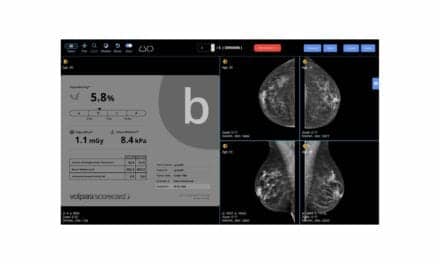
To test visual hindsight bias among expert breast radiologists, the researchers used “repeated imaging with single evaluation,” also known as the RISE method. RISE consists of presenting the subjects with images that repeat in an unpredictable order with varying levels of noise throughout the experiment. This ensures that the effects of any biases are truly visual rather than cognitive.
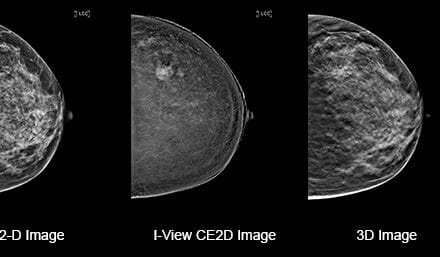
In their study, the team recruited 34 expert radiologists and subjected them to multiple series of mammograms with abnormalities using RISE. In some of these series (blocks), the mammograms were very blurry at first and became clearer as the trial proceeded. In other blocks, the mammograms were clear first and then degraded in quality with time. For each of the mammograms shown, the radiologists were asked to decide whether the abnormality in the image corresponded to a mass or a calcification and state how confident they were in their assessment.
The researchers hypothesized that radiologists seeing clearer, noise-free images first should be able to respond more accurately and confidently for the blurry versions of the same images owing to visual hindsight bias. The experimental findings indeed supported this hypothesis, as radiologists observing an image without added noise performed significantly better for the noisiest versions of that same image. This result showed how prior information gained from viewing the clearer images allowed radiologists to assess noisy images more accurately when the visual input was weak.
“This paper suggests that the phenomenon of ‘missed’ lesions on a previous mammogram subsequently found ‘in hindsight’ by another radiologist after diagnosis is an effect of the visual hindsight bias and not only a decision-level error,” says Professor Maryellen L. Giger, PhD, JMI’s editor in chief. “The results of this paper have implications for not only negligence lawsuits against radiologists but also the general population of patients who wonder ‘what if the lesion had been found earlier?’”
Feature image: Expert radiologists interpret mammogram image details as breast calcifications or abnormal masses with varying degrees of confidence and accuracy. Hindsight bias plays an important role.