Researchers at Sylvester Comprehensive Cancer Center in Miami are looking at ways to combine imaging and biomarkers to predict prostate cancer progression more accurately. The study was part of a National Cancer Institute (NCI)-funded prospective trial of men who are monitoring their prostate cancer in a management process called active surveillance. Results were recently published in the Journal of Urology.
Some prostate cancers grow slowly and are unlikely to result in any long-term consequence. As a result, many men with prostate cancer are at risk for overtreatment and related side effects. As a result, active surveillance has emerged as an increasingly popular option for the management of prostate cancer.
“MRI of the prostate and tissue-based genomic markers are two of the new technologies that have emerged over the past few years to improve decision making and risk prediction for men who are watching their cancers for progression,” says principal investigator Sanoj Punnen, MD, co-chair of the Genitourinary Site Disease Group at Sylvester and associate professor of urology at the University of Miami Miller School of Medicine.
“This trial, called the MRI-guided Active Selection for Treatment of Prostate Cancer [Miami MAST] trial, adds clarity to how these new tests might be used to improve the selection and monitoring of men considering surveillance,” Punnen adds.
A New Tool for Detection and Risk Assessment
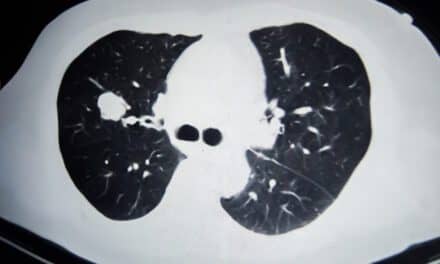
Punnen and colleagues started the MAST study in 2014, when MRI of the prostate was emerging as one of the newest tools for detecting prostate cancer and assessing its risk. “Before MRI, we did not have a reliable way to image the prostate to distinguish between benign prostate growths and cancer,” Punnen says. Typically, men who have a high prostate specific antigen (PSA) test get a prostate biopsy to check for cancer.”
“We do the biopsy by taking samples of the gland in 10 to 12 different areas. If only one or two of those cores come back with a low-grade cancer, then the patient likely does not yet need treatment and we monitor the cancer,” Punnen says.
One of the big concerns with active surveillance is that while most patients do well with surveillance, initial biopsy results underestimate patients’ risk for cancer progression in a small percentage of patients. As a result, many providers will perform a prostate biopsy every year to evaluate for progression.
“That can be burdensome for the patient,” Punnen says. “In the MAST study, the NCI grant paid for each patient in the trial to get a biopsy and MRI every year for the first three years. Overall, from the time a man is diagnosed to the time he comes off this trial, we have about five years of data on each patient.”
Punnen adds, “Within this time, we have serial imaging of the prostate on MRI, pathology data from serial biopsy, and molecular information from serial blood and urine tests that we can relate to the risk of tumor progression to learn how to better tailor the intensity of each surveillance program to the individual’s personalized risk of cancer progression.”
While MRI has played an increasing role in the detection of prostate cancer, its role in active surveillance is less clear. Furthermore, MRI is subjective and can miss anywhere from 10% to 30% of clinically significant cancers.
Genomic Signatures Aid Prediction
Genetic information from biopsy tissue, as well as blood and urine samples, adds another layer of risk stratification to help inform decision-making. Sylvester researchers have been evaluating the value of adding genetics data focused on genes or signatures that may suggest risk for more aggressive cancer.
“Many scientists have suggested these genomic signatures may be more predictive than cancer grade in predicting how aggressive the cancer will be,” Punnen says. “Part of our work in the MAST study has been collaborating with one of the biggest genomic vendors in this space to analyze the genomics from prostate cancer biopsy tissue from men on the trial.”
One of the issues with genomic testing is that the test is conducted only on a single core with the highest-grade cancer. However, prostate cancer is multi-focal and heterogeneous and the core with the highest grade may not always represent the core with the highest genomic risk.
Punnen and his team combined data from the MAST trial and another prostate cancer trial in radiation oncology (the BlaStM trial) and reported that the cancer with the highest grade tends to have the highest genomic risk in more than 80% of the cases. However, nearly 20% of cases found the worst genomic risk in a cancer of lower grade that would not have been analyzed per standard of care.
“This is a novel finding that adds important information regarding the benefits and limitations of these tests in the biopsy setting,” Punnen says. The article also found that biopsy cores that were performed with MRI targeting had higher genomic risks than biopsy cores that were performed without MRI targeting.
“We believe the Journal accepted our work because it provides something new about how we can use these signatures and what we need to be aware of,” Punnen says. “At this point, we know using the MRI is going to enhance patient surveillance, but now we have all these different data points at the genomic and molecular level on men that are monitoring their tumors to detect change.”
The combination of data points is an evolution in precision medicine that might eventually improve prostate cancer risk stratification in all men considering prostate cancer surveillance. Punnen and colleagues recently received a five-year $2.9 million NCI grant to study how an artificial intelligence algorithm applied to prostate MRI could further improve prostate cancer risk evaluation.