Estimated to become the second leading cause of cancer deaths in the U.S. by 2030, pancreatic cancer has a grim prognosis with nearly 70% of patients facing mortality within the first year of diagnosis. Unfortunately, 40% of small pancreatic cancers elude detection on CT scans until they’ve advanced to an incurable stage.
This creates a critical “last-mile” barrier for early detection efforts where, in most patients—including those high-risk subjects undergoing active screening—imaging detects the cancer at a stage when a cure is unlikely. This makes imaging the final frontier in the quest for early cancer detection.
In a recent breakthrough, Mayo Clinic Comprehensive Cancer Center researchers used the world’s most extensive imaging dataset to build a versatile artificial intelligence (AI) model that has shown the potential for autonomous detection of pancreatic cancer on standard CTs when surgical intervention can still promise a cure.
“This is where the study emerges as a beacon of hope,” says Ajit H. Goenka, MD., a Mayo Clinic radiologist and principal investigator and corresponding author. “It addresses the last-mile challenge—detecting the cancer at a stage when the cancer is even beyond the scope of experts.”
The group developed a highly accurate AI model, trained on the largest—more than 3,000 patients—and most diverse CT dataset, for fully automated cancer detection, including small and otherwise difficult-to-detect tumors. Published in Gastroenterology, the journal of the American Gastroenterological Association, the study not only builds on the group’s recent work on radiomics-based early detection models but also underscores Mayo Clinic’s standing as a beacon of innovation in AI healthcare solutions.
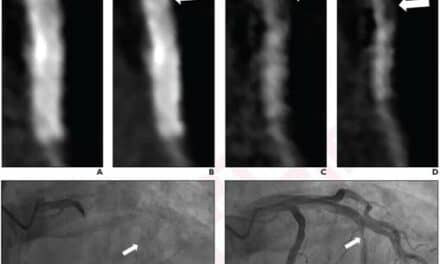
Most important, the model could detect visually imperceptible cancer from normal-appearing pancreases on prediagnostic CT images (i.e., those acquired at three to 36 months prior to clinical diagnosis) substantially early—a median of 438 days—before clinical diagnosis.
“These findings suggest that AI has the potential to detect hidden cancers in asymptomatic individuals, allowing for surgical treatment at a stage when a cure is still achievable,” Goenka says.
Finally, the model remained reliable and accurate across diverse patient groups and variations in scanning equipment and imaging techniques. This resilience is crucial for the model’s utility in a wide array of real-world medical scenarios.
Addressing a major concern in the AI healthcare landscape, the team also deconstructed the AI’s decision-making process to ensure transparency, acknowledging that trust and quality control are essential for AI’s broader clinical acceptance.
“We owe the progress to the ingenious efforts of the Framework for AI Software Technology, or FAST, team led by Panagiotis Korfiatis, PhD, complemented by our team of exceptionally bright research fellows and data science analysts,” says Goenka. “They dedicated months to meticulous preparation for our initial submission and invested significant effort to astutely address the incisive queries of the panel of international reviewers.”
“We’re only at the beginning but stand ready to address the challenges of early cancer detection, leveraging the capabilities of AI and next-generation molecular imaging in conjunction with complementary biomarkers,” he adds.
Mayo Clinic has already initiated the steps for clinical validation and the models are undergoing regulatory processes. With backing from the Mayo Clinic Comprehensive Cancer Center, the team is set to undertake benefactor-funded prospective screening trials. The insights from these trials will refine and bolster the practical effectiveness of their innovative approach.